FAQs
What is
Prostate Cancer?


Early-stage prostate cancer often has no symptoms. As the cancer progresses, symptoms may include:
– Difficulty starting or stopping the flow of urine
– Weak or interrupted flow of urine
– Frequent urination, especially at night
– Painful or burning urination
– Difficulty getting an erection
– Painful ejaculation
– Blood in urine or semen
The exact cause of prostate cancer is unknown, but risk factors include:
– Age (risk increases after 50)
– Family history (having a father or brother with prostate cancer)
– Race (African American men have a higher risk)
Men with the following risk factors should be screened regularly:
– Age 50 or older
– African American men
– Men with a family history of prostate cancer
– Men with a history of prostate issues (e.g., enlarged prostate)
Diagnosis typically involves:
– PSA (prostate-specific antigen) test: measures protein levels in blood
– Digital rectal exam (DRE): doctor examines the prostate gland manually
– Biopsy: tissue sample is taken from the prostate gland for examination
The PSA test measures the level of prostate-specific antigen (PSA) in the blood. Elevated PSA levels can indicate prostate issues, including cancer.
Treatment options depend on the stage and aggressiveness of the cancer:
– Surgery (prostatectomy): removal of the prostate gland
– Radiation therapy: high-energy rays to kill cancer cells
– Active surveillance: regular monitoring without immediate treatment
– Hormone therapy: reducing androgen hormones to slow cancer growth
A prostatectomy is a surgical procedure to remove the prostate gland. There are two main types:
– Radical prostatectomy: removes the entire prostate gland
– Laparoscopic prostatectomy: minimally invasive surgery using a laparoscope
Radiation therapy uses high-energy rays to kill cancer cells. There are two main types:
– External beam radiation therapy (EBRT): radiation is delivered from outside the body
– Brachytherapy: radiation is delivered from inside the body using implanted seeds
Active surveillance is a treatment approach that involves regular monitoring and testing, including PSA tests and biopsies, to track the progression of the cancer without immediate treatment.
While there is no sure way to prevent prostate cancer, a healthy diet and regular exercise may help reduce the risk.
The 5-year survival rate for prostate cancer is high, around 92%, due to early detection and effective treatment.
Yes, prostate cancer can recur after treatment. Regular monitoring and follow-up appointments with a doctor are essential to detect any recurrences early.
Men with risk factors should get screened annually, starting at age 50. Men without risk factors should discuss screening with their doctor.
The impact of prostate cancer treatment on fertility depends on the type of treatment. Surgery and radiation therapy may affect fertility, while hormone therapy may not. Men should discuss their fertility options with their doctor before treatment.
What is
Ovarian Cancer?

Ovarian cancer is a type of cancer that affects the ovaries, which are the organs that produce eggs in women. It occurs when abnormal cells in the ovaries grow and multiply uncontrollably, forming a tumor.

Early-stage ovarian cancer often has no symptoms. As the cancer progresses, symptoms may include:
– Abdominal pain or discomfort
– Bloating or swelling in the abdomen
– Pelvic pain or pressure
– Abnormal vaginal bleeding or discharge
– Difficulty eating or feeling full quickly
– Urinary frequency or urgency
The exact cause of ovarian cancer is unknown, but risk factors include:
– Genetic mutations (BRCA1 and BRCA2 genes)
– Family history of ovarian or breast cancer
– Reproductive issues (endometriosis, polycystic ovary syndrome)
– Hormone replacement therapy
Women with the following risk factors should be screened regularly:
– BRCA1 or BRCA2 genetic mutation
– Family history of ovarian or breast cancer
– Reproductive issues (endometriosis, polycystic ovary syndrome)
– Age 55 or older
Diagnosis typically involves:
– Pelvic exam: doctor examines the ovaries and uterus manually
– Ultrasound: uses sound waves to create images of the ovaries
– CA-125 blood test: measures protein levels in blood
– Biopsy: tissue sample is taken from the ovary for examination
The CA-125 test measures the level of a protein called cancer antigen 125 in the blood. Elevated levels can indicate ovarian cancer.
Treatment options depend on the stage and aggressiveness of the cancer:
– Surgery: removes tumor, ovaries, fallopian tubes, and uterus
– Chemotherapy: drugs to kill cancer cells
– Radiation therapy: high-energy rays to kill cancer cells
– Targeted therapy: drugs to target specific cancer cells
The goal of surgery is to remove the tumor, ovaries, fallopian tubes, and uterus to prevent the cancer from spreading.
Chemotherapy uses drugs to kill cancer cells. It can be given orally or intravenously.
While there is no sure way to prevent ovarian cancer, birth control pills and tubal ligation may reduce the risk.
The 5-year survival rate for ovarian cancer is around 49%, depending on the stage and treatment.
Yes, ovarian cancer can recur after treatment. Regular monitoring and follow-up appointments with a doctor are essential.
Annual screening is recommended for high-risk women, including those with a family history or genetic mutation.
Depends on the type of treatment and individual situation. Some treatments may affect fertility.
Genetic testing identifies BRCA1 and BRCA2 genes, which increase ovarian cancer risk. Knowing your genetic status can help guide screening and prevention decisions.
What is
Colon Cancer?

Colon cancer, also known as colorectal cancer, is a type of cancer that affects the colon (large intestine) or rectum (the last part of the colon). It occurs when abnormal cells in the colon or rectum grow and multiply uncontrollably, forming a tumor. Over time, the tumor can invade the wall of the colon or rectum and spread to other parts of the body.

Early-stage colon cancer often has no symptoms. As the cancer progresses, symptoms may include:
– Blood in stool (hematochezia)
– Changes in bowel movements (diarrhea or constipation)
– Abdominal pain or cramping
– Weakness and fatigue
– Loss of appetite
– Narrow stools
– Feeling of incomplete evacuation
– Abdominal distension
The exact cause of colon cancer is unknown, but risk factors include:
– Age (over 50)
– Family history of colon cancer or polyps
– Diet high in processed meat and low in fiber
– Inflammatory bowel disease (IBD)
– Obesity
– Smoking
– Alcohol consumption
– Lack of physical activity
Adults over 50, those with a family history of colon cancer or polyps, and individuals with IBD or obesity are at increased risk. Additionally, people with a history of smoking, alcohol consumption, or a sedentary lifestyle are also at higher risk.
Diagnosis typically involves:
– Colonoscopy: a procedure to examine the colon with a flexible tube called a colonoscope
– Flexible sigmoidoscopy: a procedure to examine the lower colon
– CT scan: a scan to create images of the colon
– Biopsy: a tissue sample is taken from the colon for examination
– Blood tests: to check for biomarkers like carcinoembryonic antigen (CEA)
A colonoscopy is a procedure to examine the colon with a flexible tube called a colonoscope. The doctor can visualize the inside of the colon, remove any polyps or tissue samples, and perform a biopsy.
Treatment options depend on the stage and aggressiveness of the cancer and include:
– Surgery: to remove the tumor and affected portion of colon
– Chemotherapy: drugs to kill cancer cells
– Radiation therapy: high-energy rays to kill cancer cells
– Targeted therapy: drugs to target specific cancer cells
– Immunotherapy: drugs to stimulate the immune system
– Palliative care: to relieve symptoms and improve quality of life
The goal of surgery is to remove the tumor and affected portion of colon to prevent the cancer from spreading. The type of surgery depends on the stage and location of the cancer.
Chemotherapy uses drugs to kill cancer cells and can be given orally or intravenously. It can be used before or after surgery, or as a standalone treatment.
Yes, colon cancer can be prevented with:
– Screening (colonoscopy)
– Healthy diet (high in fiber, low in processed meat)
– Lifestyle changes (regular exercise, weight management)
– Avoiding smoking and alcohol consumption
The 5-year survival rate for colon cancer is around 65%, depending on the stage and treatment. Early detection improves survival rates.
Yes, colon cancer can recur after treatment. Regular monitoring and follow-up appointments with a doctor are essential to detect any recurrences early.
Annual screening is recommended for adults over 50, or earlier if there is a family history or other risk factors.
Yes, most people can resume normal activities after treatment. However, some may experience lingering effects like bowel changes or fatigue.
Early detection improves treatment outcomes and survival rates. It also reduces the risk of complications and improves quality of life.
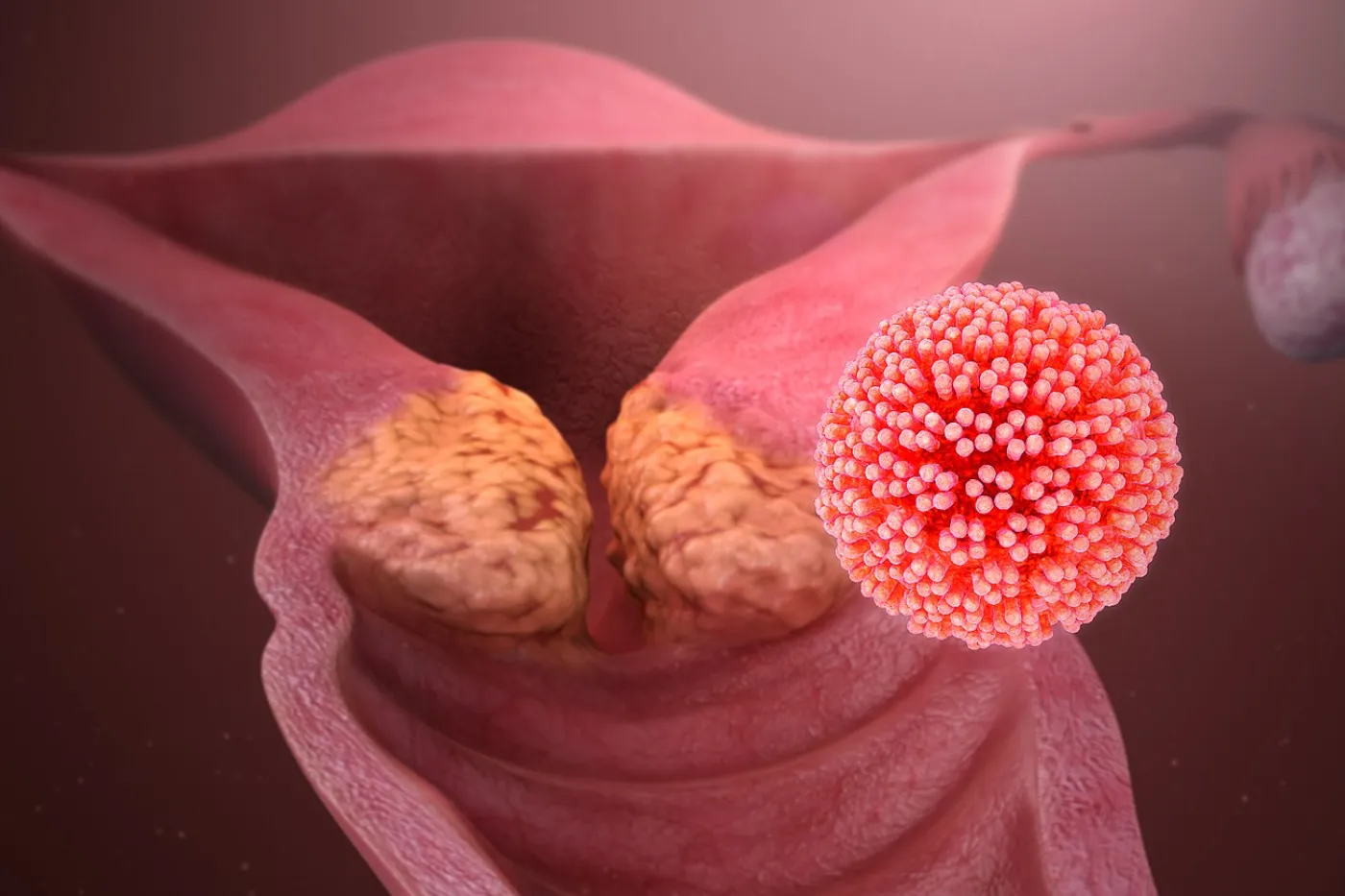
What is
Cervical Cancer?

Cervical cancer is a type of cancer that affects the cervix, the lower part of the uterus (womb). It occurs when abnormal cells in the cervix grow and multiply uncontrollably, forming a tumor. Over time, the tumor can invade the surrounding tissues and spread to other parts of the body.

Early-stage cervical cancer often has no symptoms. However, as the cancer progresses, symptoms may include:
– Abnormal vaginal bleeding (e.g., bleeding between periods, after sex, or after menopause)
– Pelvic pain or discomfort
– Painful urination or defecation
– Unusual vaginal discharge (e.g., bloody, watery, or foul-smelling)
– Postcoital bleeding (bleeding after sexual intercourse)
– Unexplained weight loss
The main cause of cervical cancer is the human papillomavirus (HPV). HPV is a common sexually transmitted infection that can cause genital warts and cervical cancer. There are over 100 types of HPV, but types 16 and 18 are most commonly associated with cervical cancer.
Women who have had sexual contact, have a weakened immune system, or have a history of cervical dysplasia (abnormal cell changes in the cervix) are at increased risk. Other risk factors include:
– Early sexual activity
– Multiple sexual partners
– Smoking
– Family history of cervical cancer
– History of other cancers (e.g., vulvar, vaginal, or anal cancer)
Diagnosis typically involves:
– Pap test (Pap smear): a procedure to collect cells from the cervix to check for abnormal cell changes
– HPV test: a test to check for the presence of HPV in the cervix
– Colposcopy: a procedure to examine the cervix with a special microscope
– Biopsy: a procedure to remove a tissue sample from the cervix for examination
A Pap test, also known as a Pap smear, is a procedure to collect cells from the cervix to check for abnormal cell changes. The test can detect:
– Normal cells
– Atypical cells (abnormal cells that may become cancerous)
– Cancer cells
The HPV test checks for the presence of HPV in the cervix. The test can detect:
– High-risk HPV types (e.g., HPV 16 and 18)
– Low-risk HPV types (e.g., HPV 6 and 11)
Treatment options depend on the stage and aggressiveness of the cancer and include:
– Surgery (e.g., hysterectomy, radical trachelectomy)
– Chemotherapy
– Radiation therapy
– Targeted therapy (e.g., bevacizumab)
– Immunotherapy (e.g., pembrolizumab)
The goal of surgery is to remove the tumor and affected tissue to prevent the cancer from spreading. The type of surgery depends on the stage and location of the cancer.
Yes, cervical cancer can be prevented with:
– Regular screening (Pap test and HPV test)
– HPV vaccination (e.g., Gardasil, Cervarix)
– Practicing safe sex (e.g., using condoms)
– Avoiding smoking and secondhand smoke
The 5-year survival rate for cervical cancer is around 66%, depending on the stage and treatment. Early detection improves survival rates.
Yes, cervical cancer can recur after treatment. Regular monitoring and follow-up appointments with a doctor are essential to detect any recurrences early.
Yes, most women can resume normal activities after treatment. However, some may experience lingering effects like vaginal dryness or painful urination.
Early detection improves treatment outcomes and survival rates. It also reduces the risk of complications and improves quality of life. Regular screening and HPV vaccination can help prevent cervical cancer and detect it early, when it is most treatable.
What is
Oral Cavity Cancer?

Oral cavity cancer, also known as mouth cancer, is a type of cancer that affects the oral cavity, including the lips, tongue, cheeks, floor of the mouth, and hard palate. It occurs when abnormal cells in the oral cavity grow and multiply uncontrollably, forming a tumor.

Early-stage oral cavity cancer often has no symptoms. As the cancer progresses, symptoms may include:
– Pain or difficulty swallowing
– Pain or difficulty speaking
– Pain or difficulty moving the tongue or jaw
– Unusual lumps or swelling in the mouth
– Unusual bleeding or pain in the mouth
– Loose teeth or dentures
– Difficulty chewing or swallowing
– Unusual changes in the voice
The main cause of oral cavity cancer is tobacco use, including smoking and chewing tobacco. Other risk factors include:
– Heavy alcohol consumption
– Human papillomavirus (HPV) infection
– Family history of oral cavity cancer
– Poor oral hygiene
– Poor diet
– Exposure to radiation therapy
Individuals who use tobacco, consume excessive alcohol, have a history of HPV infection, or have a family history of oral cavity cancer are at increased risk. Men are more likely to develop oral cavity cancer than women.
Diagnosis typically involves:
– Visual examination of the oral cavity
– Biopsy (removing a tissue sample for examination)
– Imaging tests (e.g., X-rays, CT scans, MRI scans)
Treatment options depend on the stage and aggressiveness of the cancer and include:
– Surgery (e.g., tumor resection, neck dissection)
– Radiation therapy
– Chemotherapy
– Targeted therapy
– Immunotherapy
The goal of surgery is to remove the tumor and affected tissue to prevent the cancer from spreading.
Yes, oral cavity cancer can be prevented by:
– Avoiding tobacco use
– Limiting alcohol consumption
– Practicing good oral hygiene
– Getting regular dental check-ups
– Avoiding exposure to radiation therapy
– Getting vaccinated against HPV
The 5-year survival rate for oral cavity cancer is around 66%, depending on the stage and treatment. Early detection improves survival rates.
Yes, oral cavity cancer can recur after treatment. Regular monitoring and follow-up appointments with a doctor are essential to detect any recurrences early.
Annual screening is recommended for individuals aged 18-65, or earlier if there is a history of oral cavity cancer or other risk factors.
Yes, most individuals can resume normal activities after treatment. However, some may experience lingering effects like difficulty speaking or swallowing.
Early detection improves treatment outcomes and survival rates. It also reduces the risk of complications and improves quality of life.
You can reduce your risk by avoiding tobacco use, limiting alcohol consumption, practicing good oral hygiene, getting regular dental check-ups, avoiding exposure to radiation therapy, and getting vaccinated against HPV.
You can get more information from your doctor, dentist, or organizations like the American Cancer Society, Oral Cancer Foundation, and National Institute of Dental and Craniofacial Research.
What is
Blood Cancer?

Blood cancer, also known as hematologic cancer, is a type of cancer that affects the blood and bone marrow. It occurs when abnormal cells in the blood or bone marrow grow and multiply uncontrollably, disrupting normal blood function.
– Leukemia: cancer of the white blood cells
– Lymphoma: cancer of the immune system
– Multiple myeloma: cancer of the plasma cells
– Myeloproliferative neoplasms: group of disorders that affect the bone marrow
– Myelodysplastic syndrome: condition where the bone marrow does not produce enough healthy blood cells
– Fatigue
– Shortness of breath
– Easy bruising or bleeding
– Pale skin
– Enlarged lymph nodes
– Unusual infections
– Weight loss
– Bone pain
– Abnormal blood cell counts
– Genetic mutations
– Exposure to radiation or chemicals
– Family history
– Previous cancer treatment
– Certain medical conditions (e.g., myelodysplastic syndrome)
– Individuals with a family history of blood cancer
– Previous cancer treatment
– Certain medical conditions (e.g., myelodysplastic syndrome)
– Genetic mutations
– Exposure to radiation or chemicals
– Physical examination
– Blood tests (e.g., complete blood count, blood chemistry tests)
– Bone marrow biopsy
– Imaging tests (e.g., X-rays, CT scans, PET scans)
– Chemotherapy
– Radiation therapy
– Targeted therapy
– Immunotherapy
– Stem cell transplantation
– Supportive care (e.g., blood transfusions, antibiotics)
– Control the cancer
– Manage symptoms
– Improve quality of life
– Cure the cancer (depending on the type and stage)
– Some types of blood cancer can be cured with treatment
– Others may require ongoing management
– Prognosis and potential for cure depend on the type and stage of cancer, as well as the individual’s overall health
– 5-year survival rate varies depending on the type and stage of cancer
– Ranges from around 20% to over 90%
– Yes, blood cancer can recur after treatment
– Regular monitoring and follow-up appointments with a doctor are essential
– Screening is not recommended for the general population
– Individuals with a family history or other risk factors may benefit from regular check-ups with their doctor
– Yes, many individuals can resume normal activities after treatment
– Some may experience lingering effects like fatigue or an increased risk of infections
– Improves treatment outcomes and survival rates
– Reduces the risk of complications and improves quality of life
– Your doctor or hematologist
– American Cancer Society
– Leukemia & Lymphoma Society
– National Cancer Institute
What is
Anal Cancer?

Anal cancer is a type of cancer that affects the anus, which is the opening at the end of the digestive tract. It occurs when abnormal cells in the anus grow and multiply uncontrollably, forming a tumor.
Symptoms of anal cancer may include:
– Bleeding from the anus or rectum
– Pain or discomfort in the anus or rectum
– Itching or irritation in the anus
– A lump or mass in the anus or rectum
– Changes in bowel movements (e.g., diarrhea, constipation)
– Discharge or pus from the anus
– Narrowing of the stool
The exact cause of anal cancer is unknown, but certain factors can increase the risk:
– Human papillomavirus (HPV) infection
– Anal sex
– Weakened immune system (e.g., HIV/AIDS, immunosuppressive therapy)
– History of cervical, vulvar, or vaginal cancer
– Smoking
– Age (risk increases after 50)
Individuals at risk for anal cancer include:
– Men who have sex with men
– Women with a history of cervical, vulvar, or vaginal cancer
– Individuals with a weakened immune system
– Those who engage in anal sex
– Smokers
– Individuals over 50
Diagnosis typically involves:
– Physical examination
– Digital rectal examination (DRE)
– Anoscopy (examining the inside of the anus with a scope)
– Biopsy (removing a tissue sample for examination)
– Imaging tests (e.g., CT scans, MRI scans)
Treatment options depend on the stage and location of the cancer:
– Surgery (e.g., local resection, abdominoperineal resection)
– Radiation therapy
– Chemotherapy
– Targeted therapy
– Immunotherapy
– Pain management
The goal of treatment is to:
– Remove the tumor
– Prevent the cancer from spreading
– Relieve symptoms
– Improve quality of life
– Cure the cancer (depending on the stage and location)
Yes, anal cancer can be cured with treatment, especially if detected early. The prognosis and potential for cure depend on the stage and location of the cancer, as well as the individual’s overall health.
The 5-year survival rate for anal cancer is around 65%, depending on the stage and location of the cancer.
Yes, anal cancer can recur after treatment. Regular monitoring and follow-up appointments with a doctor are essential to detect any recurrences early.
Screening is not recommended for the general population, but individuals at high risk (e.g., men who have sex with men, those with a history of cervical, vulvar, or vaginal cancer) may benefit from regular screening with a digital rectal examination (DRE) and anoscopy.
Yes, many individuals can resume normal activities after treatment, but some may experience lingering effects like pain, bleeding, or changes in bowel movements.
Early detection improves treatment outcomes and survival rates, and reduces the risk of complications and improves quality of life.
You can get more information from your doctor, a colorectal surgeon, or organizations like the American Cancer Society, the National Cancer Institute, and the Anal Cancer Foundation.
Support resources include:
– Counseling
– Support groups
– Online forums and communities
– Educational resources
– Financial assistance programs
What is
Stomach Cancer?

Stomach cancer, also known as gastric cancer, is a type of cancer that affects the stomach. It occurs when abnormal cells in the stomach grow and multiply uncontrollably, forming a tumor.

Symptoms of stomach cancer may include:
– Abdominal pain or discomfort
– Nausea and vomiting
– Weight loss
– Loss of appetite
– Bloating or gas
– Difficulty swallowing
– Blood in stool or vomit
– Fatigue
The exact cause of stomach cancer is unknown, but certain factors can increase the risk:
– Infection with Helicobacter pylori (H. pylori)
– Diet high in salt and processed meat
– Smoking
– Family history
– Age (risk increases after 50)
– Gender (men are more likely to develop stomach cancer)
– Obesity
– Pernicious anemia
– Radiation exposure
Individuals at risk for stomach cancer include:
– Those infected with H. pylori
– Men over 50
– Women over 60
– Individuals with a family history
– Smokers
– Those with a diet high in salt and processed meat
– Obese individuals
– Those with pernicious anemia
– Those exposed to radiation
Diagnosis typically involves:
– Endoscopy
– Upper gastrointestinal series (UGI)
– Computed tomography (CT) scan
– Magnetic resonance imaging (MRI) scan
– Positron emission tomography (PET) scan
– Biopsy
Treatment options depend on the stage and location of the cancer:
– Surgery (e.g., gastrectomy, subtotal gastrectomy)
– Chemotherapy
– Radiation therapy
– Targeted therapy
– Immunotherapy
– Palliative care
The goal of treatment is to:
– Remove the tumor
– Prevent the cancer from spreading
– Relieve symptoms
– Improve quality of life
– Cure the cancer (depending on the stage and location)
Yes, stomach cancer can be cured with treatment, especially if detected early. The prognosis and potential for cure depend on the stage and location of the cancer, as well as the individual’s overall health.
The 5-year survival rate for stomach cancer is around 30%, depending on the stage and location of the cancer.
Yes, stomach cancer can recur after treatment. Regular monitoring and follow-up appointments with a doctor are essential to detect any recurrences early.
Screening is not recommended for the general population, but individuals at high risk (e.g., those with H. pylori infection, family history, or previous stomach cancer) may benefit from regular screening with endoscopy and biopsy.
Yes, many individuals can resume normal activities after treatment, but some may experience lingering effects like pain, nausea, or changes in appetite.
Early detection improves treatment outcomes and survival rates, and reduces the risk of complications and improves quality of life.
You can get more information from your doctor, a gastroenterologist, or organizations like the American Cancer Society, the National Cancer Institute, and the Stomach Cancer Foundation.
Support resources include:
– Counseling
– Support groups
– Online forums and communities
– Educational resources
– Financial assistance programs
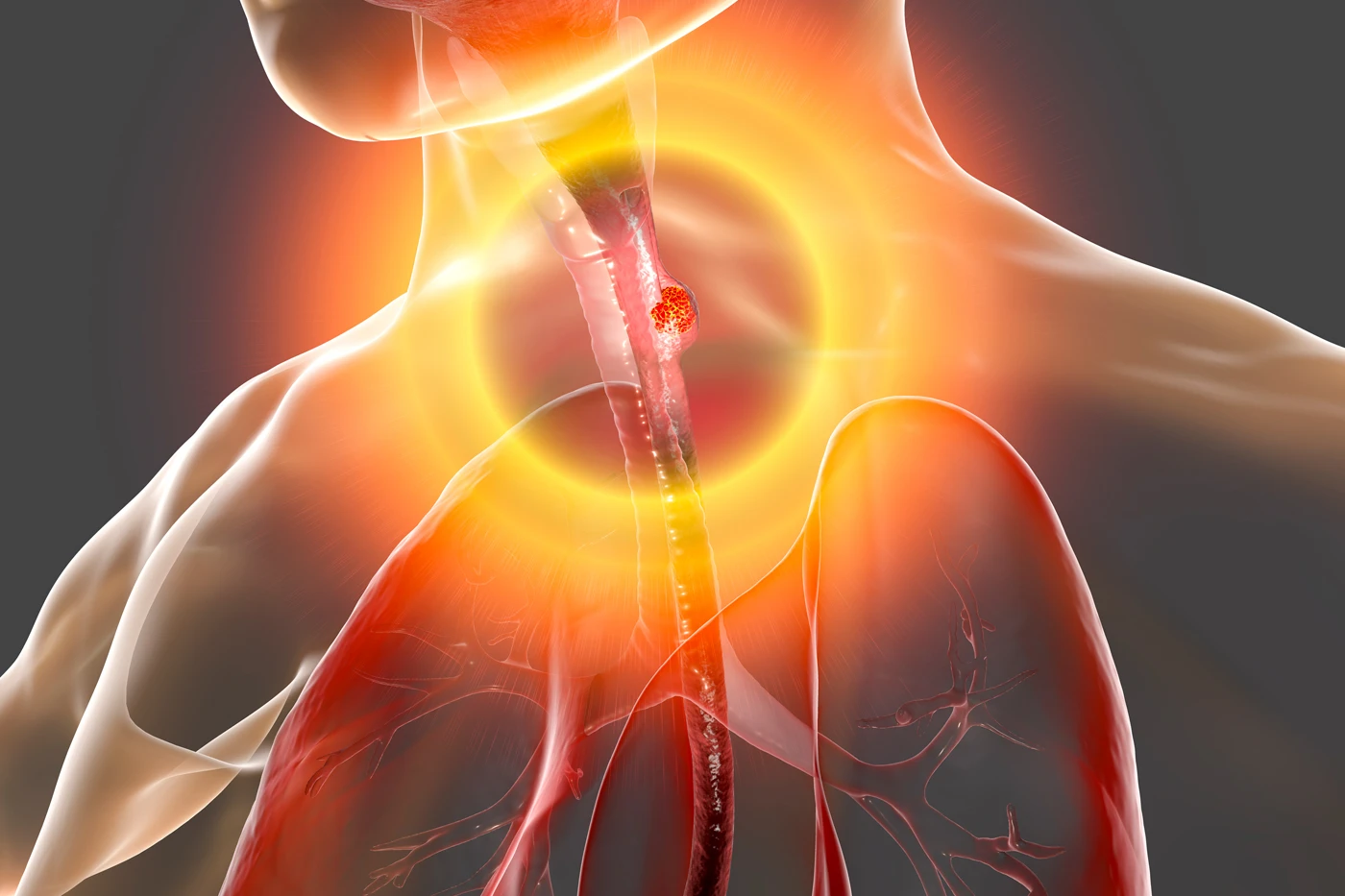
What is
Esophageal Cancer?

Esophageal cancer is a type of cancer that affects the esophagus, which is the tube that carries food and liquids from the throat to the stomach. It occurs when abnormal cells in the esophagus grow and multiply uncontrollably, forming a tumor.
Symptoms of esophageal cancer may include:
– Difficulty swallowing (dysphagia)
– Pain or discomfort in the chest or back
– Weight loss
– Coughing or choking on food
– Hoarseness
– Blood in stool or vomit
– Fatigue
The exact cause of esophageal cancer is unknown, but certain factors can increase the risk:
– Smoking
– Heavy alcohol consumption
– Gastroesophageal reflux disease (GERD)
– Barrett’s esophagus
– Family history
– Age (risk increases after 50)
– Gender (men are more likely to develop esophageal cancer)
– Obesity
– Diet high in processed meat and low in fruits and vegetables
Individuals at risk for esophageal cancer include:
– Smokers
– Heavy alcohol consumers
– Those with GERD or Barrett’s esophagus
– Men over 50
– Women over 60
– Obese individuals
– Those with a family history
– Those who eat a diet high in processed meat and low in fruits and vegetables
Diagnosis typically involves:
– Endoscopy
– Biopsy
– Computed tomography (CT) scan
– Magnetic resonance imaging (MRI) scan
– Positron emission tomography (PET) scan
– Barium swallow
Treatment options depend on the stage and location of the cancer:
– Surgery (e.g., esophagectomy, subtotal esophagectomy)
– Chemotherapy
– Radiation therapy
– Targeted therapy
– Immunotherapy
– Palliative care
The goal of treatment is to:
– Remove the tumor
– Prevent the cancer from spreading
– Relieve symptoms
– Improve quality of life
– Cure the cancer (depending on the stage and location)
Yes, esophageal cancer can be cured with treatment, especially if detected early. The prognosis and potential for cure depend on the stage and location of the cancer, as well as the individual’s overall health.
The 5-year survival rate for esophageal cancer is around 20%, depending on the stage and location of the cancer.
Yes, esophageal cancer can recur after treatment. Regular monitoring and follow-up appointments with a doctor are essential to detect any recurrences early.
Screening is not recommended for the general population, but individuals at high risk (e.g., those with GERD or Barrett’s esophagus) may benefit from regular screening with endoscopy and biopsy.
Early detection improves treatment outcomes and survival rates, and reduces the risk of complications and improves quality of life.
You can get more information from your doctor, a gastroenterologist, or organizations like the American Cancer Society, the National Cancer Institute, and the Esophageal Cancer Foundation.
Support resources include:
– Counseling
– Support groups
– Online forums and communities
– Educational resources
– Financial assistance programs
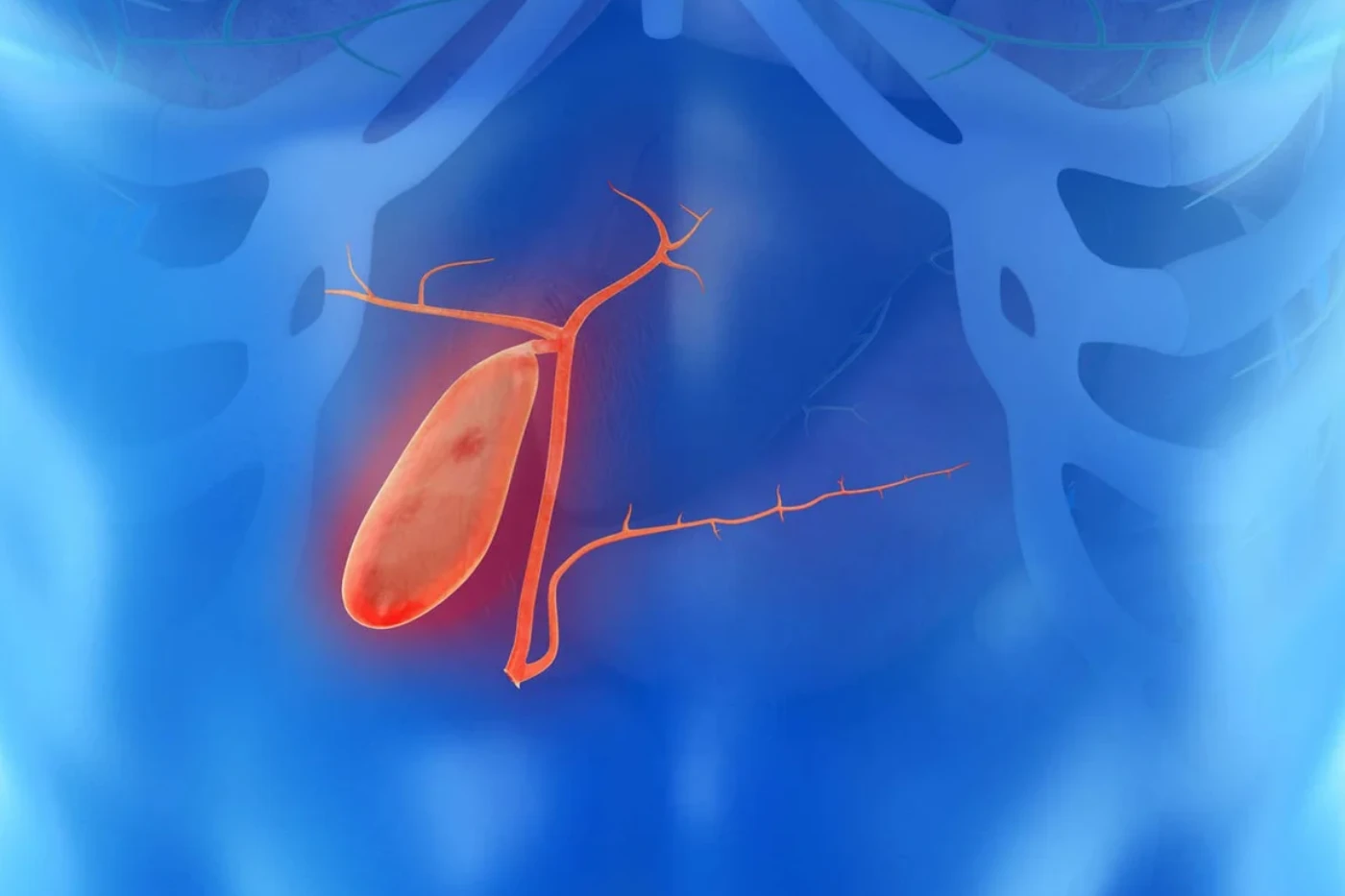
What is
Gallbladder Cancer?

Gallbladder cancer is a type of cancer that affects the gallbladder, a small organ located under the liver that stores bile. It occurs when abnormal cells in the gallbladder grow and multiply uncontrollably, forming a tumor.
Symptoms of gallbladder cancer may include:
– Abdominal pain (especially in the right upper quadrant)
– Nausea and vomiting
– Weight loss
– Loss of appetite
– Jaundice (yellowing of the skin and eyes)
– Pale or clay-colored stools
– Dark urine
– Fever
– Shaking chills
The exact cause of gallbladder cancer is unknown, but certain factors can increase the risk:
– Gallstones
– Choledochal cysts
– Primary sclerosing cholangitis
– Ulcerative colitis
– Family history
– Age (risk increases after 50)
– Gender (women are more likely to develop gallbladder cancer)
– Obesity
– Diabetes
– High cholesterol
Individuals at risk for gallbladder cancer include:
– Those with a history of gallstones
– Those with choledochal cysts
– Those with primary sclerosing cholangitis
– Those with ulcerative colitis
– Women over 50
– Obese individuals
– Those with diabetes
– Those with high cholesterol
– Those with a family history
Diagnosis typically involves:
– Physical examination
– Medical history
– Laboratory tests (e.g., liver function tests, tumor markers)
– Imaging tests (e.g., ultrasound, CT scan, MRI scan)
– Biopsy
Treatment options depend on the stage and location of the cancer:
– Surgery (e.g., cholecystectomy, radical cholecystectomy)
– Chemotherapy
– Radiation therapy
– Targeted therapy
– Immunotherapy
– Palliative care
The goal of treatment is to:
– Remove the tumor
– Prevent the cancer from spreading
– Relieve symptoms
– Improve quality of life
– Cure the cancer (depending on the stage and location)
Yes, gallbladder cancer can be cured with treatment, especially if detected early. The prognosis and potential for cure depend on the stage and location of the cancer, as well as the individual’s overall health.
The 5-year survival rate for gallbladder cancer is around 20%, depending on the stage and location of the cancer.
Yes, gallbladder cancer can recur after treatment. Regular monitoring and follow-up appointments with a doctor are essential to detect any recurrences early.
Screening is not recommended for the general population, but individuals at high risk (e.g., those with gallstones or choledochal cysts) may benefit from regular screening with ultrasound and laboratory tests.
Yes, many individuals can resume normal activities after treatment, but some may experience lingering effects like abdominal pain or jaundice.
Early detection improves treatment outcomes and survival rates, and reduces the risk of complications and improves quality of life.
You can get more information from your doctor, a gastroenterologist, or organizations like the American Cancer Society, the National Cancer Institute, and the Gallbladder Cancer Foundation.
Support resources include:
– Counseling
– Support groups
– Online forums and communities
– Educational resources
– Financial assistance programs
What is
Urinary Bladder Cancer?

Urinary bladder cancer is a type of cancer that affects the urinary bladder, a hollow organ that stores urine. It occurs when abnormal cells in the bladder grow and multiply uncontrollably, forming a tumor.

Symptoms of urinary bladder cancer may include:
– Blood in the urine (hematuria)
– Painful urination (dysuria)
– Frequent urination
– Urgent need to urinate
– Pain in the lower abdomen or back
– Weakness or fatigue
– Loss of appetite
– Weight loss
The exact cause of urinary bladder cancer is unknown, but certain factors can increase the risk:
– Smoking
– Exposure to chemicals (e.g., benzene, arsenic)
– Radiation therapy
– Family history
– Age (risk increases after 50)
– Gender (men are more likely to develop bladder cancer)
– Race (whites are more likely to develop bladder cancer)
– Chronic bladder inflammation
– Bladder birth defects
Individuals at risk for urinary bladder cancer include:
– Smokers
– Those exposed to chemicals (e.g., benzene, arsenic)
– Those with a family history
– Men over 50
– Women over 50
– Whites
– Those with chronic bladder inflammation
– Those with bladder birth defects
Diagnosis typically involves:
– Physical examination
– Medical history
– Laboratory tests (e.g., urinalysis, blood tests)
– Imaging tests (e.g., ultrasound, CT scan, MRI scan)
– Cystoscopy
– Biopsy
Treatment options depend on the stage and location of the cancer:
– Surgery (e.g., transurethral resection of bladder tumor, radical cystectomy)
– Chemotherapy
– Radiation therapy
– Immunotherapy
– Targeted therapy
– Palliative care
The goal of treatment is to:
– Remove the tumor
– Prevent the cancer from spreading
– Relieve symptoms
– Improve quality of life
– Cure the cancer (depending on the stage and location)
Yes, urinary bladder cancer can be cured with treatment, especially if detected early. The prognosis and potential for cure depend on the stage and location of the cancer, as well as the individual’s overall health.
The 5-year survival rate for urinary bladder cancer is around 70%, depending on the stage and location of the cancer.
Yes, urinary bladder cancer can recur after treatment. Regular monitoring and follow-up appointments with a doctor are essential to detect any recurrences early.
Screening is not recommended for the general population, but individuals at high risk (e.g., those with a history of smoking or exposure to chemicals) may benefit from regular screening with urinalysis and cystoscopy.
Yes, many individuals can resume normal activities after treatment, but some may experience lingering effects like urinary incontinence or sexual dysfunction.
Early detection improves treatment outcomes and survival rates, and reduces the risk of complications and improves quality of life.
You can get more information from your doctor, a urologist, or organizations like the American Cancer Society, the National Cancer Institute, and the Bladder Cancer Foundation.
Support resources include:
– Counseling
– Support groups
– Online forums and communities
– Educational resources
– Financial assistance programs
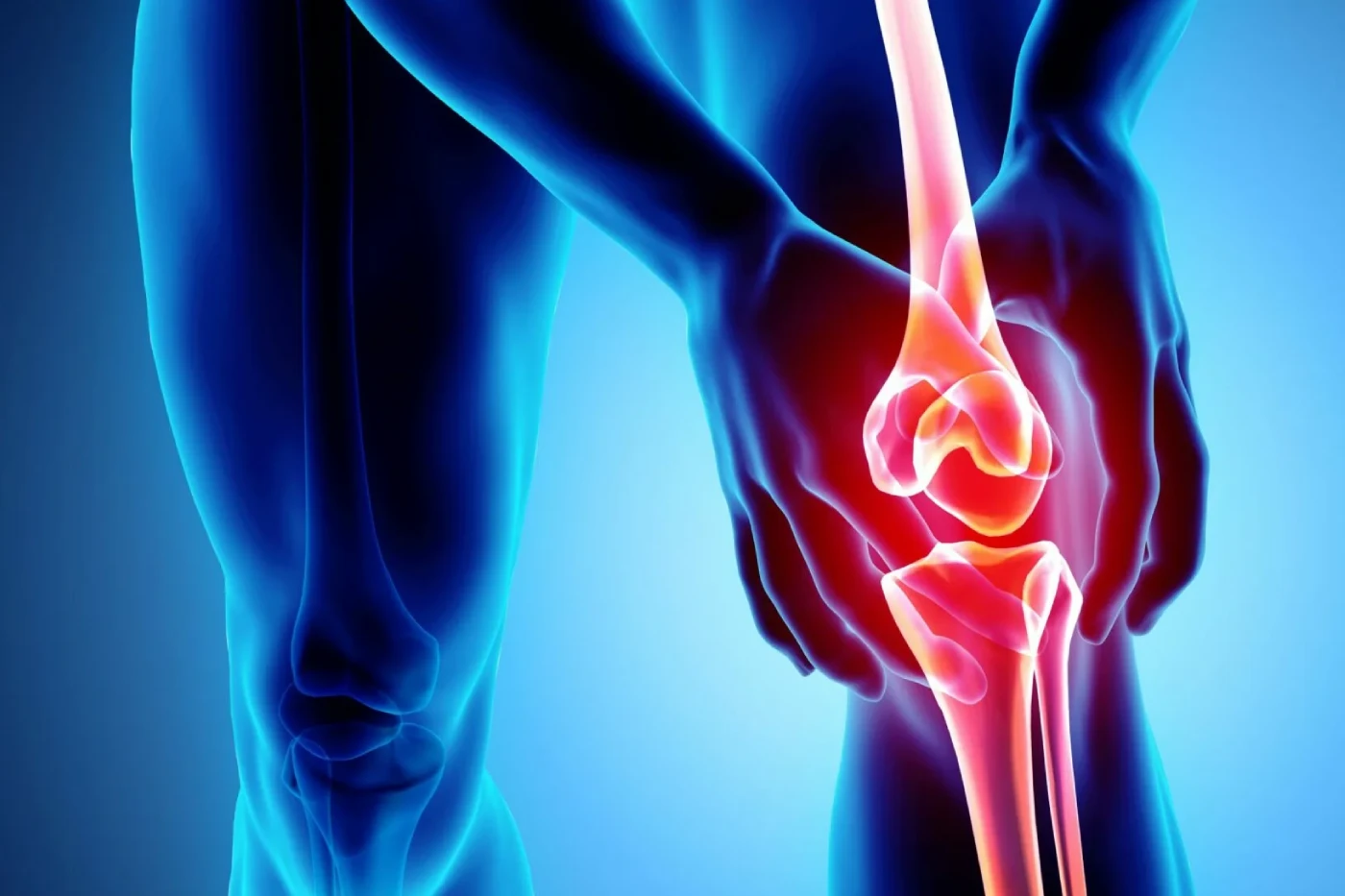
What is
Bone Cancer?

Bone cancer is a type of cancer that affects the bones. It occurs when abnormal cells in the bone grow and multiply uncontrollably, forming a tumor.
– Types of bone cancer:
Osteosarcoma, Ewing’s sarcoma, Chondrosarcoma, Fibrosarcoma, Chordoma
Symptoms of bone cancer may include:
– Pain in the affected bone
– Swelling or redness in the affected area
– Weakness or fatigue
– Difficulty moving the affected limb
– Fractures or breaks in the affected bone
– Weight loss
– Fever
– Night sweats
The exact cause of bone cancer is unknown, but certain factors can increase the risk:
– Genetic mutations
– Family history
– Radiation exposure
– Chemotherapy
– Certain bone diseases (e.g., Paget’s disease, osteochondritis)
– Inherited conditions (e.g., Li-Fraumeni syndrome, hereditary multiple exostoses)
Individuals at risk for bone cancer include:
– Those with a family history
– Those with genetic mutations
– Those who have had radiation therapy
– Those with certain bone diseases
– Those with inherited conditions
– Children and young adults (bone cancer is more common in this age group)
Diagnosis typically involves:
– Physical examination
– Medical history
– Laboratory tests (e.g., blood tests, imaging studies)
– Biopsy
Treatment options depend on the type and stage of the cancer:
– Surgery (e.g., limb-sparing surgery, amputation)
– Chemotherapy
– Radiation therapy
– Targeted therapy
– Immunotherapy
– Palliative care
The goal of treatment is to:
– Remove the tumor
– Prevent the cancer from spreading
– Relieve symptoms
– Improve quality of life
– Cure the cancer (depending on the type and stage)
Yes, bone cancer can be cured with treatment, especially if detected early. The prognosis and potential for cure depend on the type and stage of the cancer, as well as the individual’s overall health.
The 5-year survival rate for bone cancer is around 70%, depending on the type and stage of the cancer.
Screening is not recommended for the general population, but individuals at high risk (e.g., those with a family history or genetic mutation) may benefit from regular screening with imaging studies and laboratory tests.
Yes, many individuals can resume normal activities after treatment, but some may experience lingering effects like limited mobility or chronic pain.
Early detection improves treatment outcomes and survival rates, and reduces the risk of complications and improves quality of life.
You can get more information from your doctor, an orthopedic oncologist, or organizations like the American Cancer Society, the National Cancer Institute, and the Bone Cancer Foundation.
Support resources include:
– Counseling
– Support groups
– Online forums and communities
– Educational resources
– Financial assistance programs
What is
Pancreatic Cancer?

Pancreatic cancer is a type of cancer that affects the pancreas, an organ located in the abdomen that produces hormones and enzymes to aid in digestion. It occurs when abnormal cells in the pancreas grow and multiply uncontrollably, forming a tumor.

Symptoms of pancreatic cancer may include:
– Abdominal pain or discomfort
– Weight loss
– Loss of appetite
– Fatigue
– Jaundice (yellowing of the skin and eyes)
– Dark urine
– Pale or clay-colored stools
– Nausea and vomiting
– Diarrhea or constipation
– Blood clots
The exact cause of pancreatic cancer is unknown, but certain factors can increase the risk:
– Smoking
– Family history
– Age (risk increases after 50)
– Gender (men are more likely to develop pancreatic cancer)
– Race (African Americans are more likely to develop pancreatic cancer)
– Obesity
– Diabetes
– Pancreatitis (inflammation of the pancreas)
– Genetic mutations (e.g., BRCA2, p16)
Individuals at risk for pancreatic cancer include:
– Smokers
– Those with a family history
– Men over 50
– African Americans
– Obese individuals
– Those with diabetes
– Those with pancreatitis
– Those with genetic mutations
Diagnosis typically involves:
– Physical examination
– Medical history
– Laboratory tests (e.g., blood tests, imaging studies)
– Biopsy
Treatment options depend on the stage and location of the cancer:
– Surgery (e.g., Whipple procedure, distal pancreatectomy)
– Chemotherapy
– Radiation therapy
– Targeted therapy
– Immunotherapy
– Palliative care
The goal of treatment is to:
– Remove the tumor
– Prevent the cancer from spreading
– Relieve symptoms
– Improve quality of life
– Cure the cancer (depending on the stage and location)
Yes, pancreatic cancer can be cured with treatment, especially if detected early. The prognosis and potential for cure depend on the stage and location of the cancer, as well as the individual’s overall health.
The 5-year survival rate for pancreatic cancer is around 9%, depending on the stage and location of the cancer.
Yes, pancreatic cancer can recur after treatment. Regular monitoring and follow-up appointments with a doctor are essential to detect any recurrences early.
Screening is not recommended for the general population, but individuals at high risk (e.g., those with a family history or genetic mutation) may benefit from regular screening with imaging studies and laboratory tests.
Yes, many individuals can resume normal activities after treatment, but some may experience lingering effects like digestive problems or fatigue.
Early detection improves treatment outcomes and survival rates, and reduces the risk of complications and improves quality of life.
You can get more information from your doctor, a gastroenterologist, or organizations like the American Cancer Society, the National Cancer Institute, and the Pancreatic Cancer Action Network.
Support resources include:
– Counseling
– Support groups
– Online forums and communities
– Educational resources
– Financial assistance programs
What is
Breast Cancer?

Breast cancer is a type of cancer that originates in the breast tissue. It can occur in both men and women, but is more common in women. Breast cancer can be invasive or non-invasive.

– New lump or thickening in the breast or underarm area
– Change in size or shape of the breast
– Dimpling or puckering of the skin
– Redness or scaliness of the skin
– Nipple discharge or change in position
– Ductal carcinoma in situ (DCIS)
– Invasive ductal carcinoma (IDC)
– Invasive lobular carcinoma (ILC)
– Triple-negative breast cancer
– HER2-positive breast cancer
– Stage 0: Cancer is non-invasive and only in the breast ducts
– Stage I: Cancer is invasive, but only in the breast tissue
– Stage II: Cancer has spread to the lymph nodes
– Stage III: Cancer has spread to the chest wall or skin
– Stage IV: Cancer has spread to other parts of the body
– Mammogram
– Ultrasound
– MRI
– Biopsy
– Surgery (lumpectomy or mastectomy)
– Radiation therapy
– Chemotherapy
– Hormone therapy
– Targeted therapy
– To remove the tumor and affected tissue
– To remove lymph nodes for examination
– To reconstruct the breast (if desired)
– To kill cancer cells that may remain after surgery
– To reduce the risk of recurrence
– To relieve symptoms (in advanced cases)
– To kill cancer cells that may have spread
– To reduce the risk of recurrence
– To treat metastatic breast cancer
– To block the production of hormones that fuel cancer growth
– To reduce the risk of recurrence
– To treat hormone-sensitive breast cancers
– To target specific proteins or genes that contribute to cancer growth
– To block the growth of cancer cells
– To reduce the risk of recurrence
– Fatigue
– Hair loss
– Nausea and vomiting
– Pain
– Swelling
– Lymphedema
– Follow your treatment plan
– Stay hydrated
– Get enough rest
– Eat a healthy diet
– Exercise regularly
– Seek support from loved ones or support groups
– Depends on the stage and type of breast cancer
– Early detection and treatment improve survival rates
– Five-year survival rate for localized breast cancer is 99%
– Five-year survival rate for metastatic breast cancer is 29%
– Get regular mammograms
– Maintain a healthy weight
– Exercise regularly
– Limit alcohol consumption
– Avoid smoking
– Eat a healthy diet
What is
Cervix & Cervical Cancer?

The cervix is the lower part of the uterus, and cervical cancer originates in this area. It can be caused by human papillomavirus (HPV) and is more common in women aged 30-50.
– Abnormal vaginal bleeding
– Pain during sex
– Foul-smelling vaginal discharge
– Pelvic pain
– Fatigue
– Squamous cell carcinoma
– Adenocarcinoma
– Adenosquamous carcinoma
– Small cell carcinoma
– Stage I: Cancer is confined to the cervix
– Stage II: Cancer has spread to the upper part of the vagina
– Stage III: Cancer has spread to the lower part of the vagina
– Stage IV: Cancer has spread to other parts of the body
– Pap test
– HPV test
– Colposcopy
– Biopsy
– Surgery (hysterectomy or trachelectomy)
– Radiation therapy
– Chemotherapy
– Targeted therapy
– To remove the tumor and affected tissue
– To remove lymph nodes for examination
– To reconstruct the vagina (if desired)
– To kill cancer cells that may remain after surgery
– To reduce the risk of recurrence
– To relieve symptoms (in advanced cases)
– To kill cancer cells that may have spread
– To reduce the risk of recurrence
– To treat metastatic cervical cancer
– To target specific proteins or genes that contribute to cancer growth
– To block the growth of cancer cells
– To reduce the risk of recurrence
– Fatigue
– Hair loss
– Nausea and vomiting
– Pain
– Swelling
– Lymphedema
– Follow your treatment plan
– Stay hydrated
– Get enough rest
– Eat a healthy diet
– Exercise regularly
– Seek support from loved ones or support groups
– Depends on the stage and type of cervical cancer
– Early detection and treatment improve survival rates
– Five-year survival rate for localized cervical cancer is 92%
– Five-year survival rate for metastatic cervical cancer is 17%
– Get regular Pap tests
– Get vaccinated against HPV
– Practice safe sex
– Don’t smoke
– Get enough exercise
– Eat a healthy diet
– American Cancer Society
– National Cancer Institute
– Cervical Cancer Awareness Partnership
– Local support groups
– Online forums and communities
What are the risk factors
for Lung Cancer?

– Smoking
– Radon exposure
– Air pollution
– Genetic factors
– Family history
– Previous radiation therapy

– Coughing
– Chest pain
– Shortness of breath
– Wheezing
– Coughing up blood
– Fatigue
– Weight loss
– Chest X-ray
– CT scan
– PET scan
– Biopsy
– Bronchoscopy
– Fine-needle aspiration
– Stage I: Cancer is confined to the lungs
– Stage II: Cancer has spread to the lymph nodes
– Stage III: Cancer has spread to the chest wall or diaphragm
– Stage IV: Cancer has spread to other parts of the body
– Surgery
– Radiation therapy
– Chemotherapy
– Targeted therapy
– Immunotherapy
– Palliative care
– To remove the tumor and affected tissue
– To remove lymph nodes for examination
– To relieve symptoms (in advanced cases)
– To improve quality of life
– To kill cancer cells that may remain after surgery
– To reduce the risk of recurrence
– To relieve symptoms (in advanced cases)
– To improve quality of life
– To kill cancer cells that may have spread
– To reduce the risk of recurrence
– To treat metastatic lung cancer
– To improve quality of life
– To target specific proteins or genes that contribute to cancer growth
– To block the growth of cancer cells
– To reduce the risk of recurrence
– To improve quality of life
– Fatigue
– Hair loss
– Nausea and vomiting
– Pain
– Swelling
– Lymphedema
– Neuropathy
– Follow your treatment plan
– Stay hydrated
– Get enough rest
– Eat a healthy diet
– Exercise regularly
– Seek support from loved ones or support groups
– Depends on the stage and type of lung cancer
– Early detection and treatment improve survival rates
– Five-year survival rate for localized lung cancer is 59%
– Five-year survival rate for metastatic lung cancer is 5%
– Don’t smoke
– Avoid radon exposure
– Avoid air pollution
– Get vaccinated against influenza and pneumonia
– Eat a healthy diet
– Exercise regularly
– American Cancer Society
– National Cancer Institute
– Lung Cancer Alliance
– Local support groups
– Online forums and communities
– Targeted therapies
– Immunotherapies
– Personalized medicine
– Liquid biopsies
– Advanced imaging techniques
– Clinical trials
What is
Tongue Cancer?

Tongue cancer is a type of cancer that starts in the tongue, which is a vital part of our mouth that helps us speak, taste, and swallow. It can be caused by several factors, including tobacco use, alcohol consumption, human papillomavirus (HPV), and genetic factors.

The symptoms of tongue cancer can vary from person to person, but common signs include pain or discomfort in the tongue, difficulty speaking or swallowing, bleeding or ulcers on the tongue, lumps or thickening on the tongue, and loss of taste or sensation in the tongue.
There are several types of tongue cancer, including squamous cell carcinoma, adenocarcinoma, adenosquamous carcinoma, and small cell carcinoma. Each type has different characteristics and requires specific treatment approaches.
The stages of tongue cancer range from Stage I to Stage IV, depending on the extent of the cancer’s spread. Early detection and treatment are crucial for improving survival rates.
Diagnosis typically involves a biopsy, imaging tests (such as CT, MRI, or PET scans), physical examination, and endoscopy. These tests help determine the type and stage of cancer.
Treatment options include surgery, radiation therapy, chemotherapy, targeted therapy, and immunotherapy. The choice of treatment depends on the type and stage of cancer, as well as the patient’s overall health.
Surgery is often the primary treatment for tongue cancer. It involves removing the tumor and affected tissue, as well as reconstructing the tongue if necessary.
Radiation therapy uses high-energy rays to kill cancer cells that may remain after surgery or to relieve symptoms in advanced cases.
Chemotherapy uses drugs to kill cancer cells that may have spread to other parts of the body.
Side effects can include pain or discomfort in the tongue, difficulty speaking or swallowing, dry mouth, fatigue, hair loss, and other symptoms. Managing these side effects is crucial for maintaining quality of life during treatment.
Managing side effects requires a comprehensive approach, including following the treatment plan, staying hydrated, getting enough rest, eating a healthy diet, exercising regularly, and seeking support from loved ones or support groups.
The prognosis for tongue cancer depends on the stage and type of cancer, as well as the patient’s overall health. Early detection and treatment improve survival rates.
Reducing the risk of tongue cancer involves avoiding tobacco products, limiting alcohol consumption, avoiding HPV infection, eating a healthy diet, exercising regularly, and getting regular check-ups.
Resources include the American Cancer Society, National Cancer Institute, Oral Cancer Foundation, local support groups, and online forums and communities.
Research advancements include targeted therapies, immunotherapies, personalized medicine, advanced imaging techniques, and clinical trials. These developments aim to improve treatment outcomes and quality of life for patients with tongue cancer.
What is
Skin Cancer?

Skin cancer is a type of cancer that affects the skin, which is the largest organ of the body. It occurs when abnormal skin cells grow and multiply in an uncontrolled manner, forming a mass or tumor. Skin cancer can be caused by various factors, including exposure to ultraviolet (UV) radiation, genetic mutations, and weakened immune systems.

There are several types of skin cancer, including:
- Melanoma: This is the most aggressive and deadliest form of skin cancer, which originates in the pigment-producing cells called melanocytes.
- Basal cell carcinoma: This is the most common form of skin cancer, which originates in the basal cells, the lowest layer of the epidermis.
- Squamous cell carcinoma: This type of skin cancer originates in the squamous cells, which are the flat cells that make up the middle and outer layers of the epidermis.
- Merkel cell carcinoma: This is a rare and aggressive form of skin cancer, which originates in the Merkel cells, a type of cell that is found in the epidermis.
- Sebaceous gland carcinoma: This is a rare form of skin cancer, which originates in the sebaceous glands, which are the oil-producing glands in the skin.
The symptoms of skin cancer can vary depending on the type, but common signs include:
– New or changing moles
– Sores that don’t heal
– Changes in skin color or texture
– Pain or itching
– Bleeding or crusting
The stages of skin cancer range from Stage I to Stage IV, depending on the extent of the cancer’s spread.
Diagnosis typically involves:
– Physical examination
– Biopsy
– Imaging tests (such as CT or PET scans)
– Dermatoscopy
Treatment options depend on the type and stage of cancer and may include:
– Surgery
– Radiation therapy
– Chemotherapy
– Targeted therapy
– Immunotherapy
Surgery is often the primary treatment for skin cancer and involves removing the tumor and affected tissue.
Radiation therapy uses high-energy rays to kill cancer cells that may remain after surgery or to relieve symptoms in advanced cases.
Chemotherapy uses drugs to kill cancer cells that may have spread to other parts of the body.
Side effects can include:
– Pain or discomfort
– Scarring
– Fatigue
– Hair loss
– Nausea and vomiting
Managing side effects requires a comprehensive approach, including:
– Following the treatment plan
– Staying hydrated
– Getting enough rest
– Eating a healthy diet
– Exercising regularly
– Seeking support from loved ones or support groups
The prognosis for skin cancer depends on the stage and type of cancer, as well as the patient’s overall health. Early detection and treatment improve survival rates.
Reducing the risk of skin cancer involves:
– Avoiding exposure to UV radiation
– Wearing protective clothing and applying sunscreen
– Avoiding tanning beds
– Getting regular skin exams
– Avoiding smoking
– Eating a healthy diet
Resources include:
– American Cancer Society
– National Cancer Institute
– Skin Cancer Foundation
– Local support groups
– Online forums and communities
Research advancements include:
– Targeted therapies
– Immunotherapies
– Personalized medicine
– Advanced imaging techniques
– Clinical trials
What is
Immunotherapy?

Immunotherapy is a type of cancer treatment that uses the body’s own immune system to fight cancer. It works by stimulating the immune system to recognize and attack cancer cells, which are often able to evade the immune system. Immunotherapy can be used to treat various types of cancer, including melanoma, lung cancer, kidney cancer, and others.
Immunotherapy works by stimulating the immune system to recognize cancer cells as foreign and attack them. This can be done through various mechanisms, including:
- Activating immune cells, such as T cells and dendritic cells, to recognize and attack cancer cells
- Enhancing the body’s natural defenses to fight cancer
- Inhibiting the growth of cancer cells
- Inducing apoptosis (cell death) in cancer cells
There are several types of immunotherapy, including:
- Monoclonal antibodies: These are laboratory-made antibodies that are designed to target specific proteins on cancer cells.
- Checkpoint inhibitors: These are drugs that release the brakes on the immune system, allowing it to attack cancer cells more effectively.
- Cancer vaccines: These are vaccines that are designed to stimulate the immune system to recognize and attack cancer cells.
- Adoptive T cell therapy: This is a type of immunotherapy that involves removing T cells from the body, expanding them in a laboratory, and then reinfusing them to attack cancer cells.
- Oncolytic virus therapy: This is a type of immunotherapy that uses viruses to infect and kill cancer cells.
The benefits of immunotherapy include:
– Targeted treatment that spares healthy cells
– Potential for long-term cancer control
– Ability to treat multiple types of cancer
– Fewer side effects compared to traditional treatments
– Improved quality of life
Side effects of immunotherapy can include:
– Fatigue
– Fever
– Chills
– Nausea and vomiting
– Diarrhea
– Headaches
– Skin rash
– Muscle pain
– Joint pain
Immunotherapy can be administered in various ways, including:
– Intravenous infusion
– Oral medication
– Injection
– Topical application
Immunotherapy is used to:
– Treat advanced cancer
– Boost the immune system after surgery or chemotherapy
– Enhance the effectiveness of other cancer treatments
– Provide long-term cancer control
The most common cancers treated with immunotherapy are:
– Melanoma
– Lung cancer
– Kidney cancer
– Bladder cancer
– Hodgkin lymphoma
Immunotherapy can be used in combination with:
– Surgery
– Chemotherapy
– Radiation therapy
– Targeted therapy
Research advancements include:
– Personalized neoantigen-based therapies
– Combination regimens
– Targeted therapies
– Adoptive T cell therapies
– Oncolytic virus therapies
Clinical trials can be found through:
– National Cancer Institute
– American Cancer Society
– (link unavailable)
– Cancer research organizations
Eligibility criteria may include:
– Type of cancer
– Stage of cancer
– Performance status
– Previous treatments
– Age and overall health
Preparation includes:
– Consulting with a healthcare provider
– Understanding treatment options
– Managing side effects
– Maintaining a healthy lifestyle
Costs may include:
– Treatment administration
– Medication
– Hospital stays
– Follow-up care
Resources include:
– Healthcare providers
– Cancer organizations
– Online forums
– Support groups
– Clinical trial resources
About
Various cancers

Prostate cancer is a type of cancer that affects the prostate gland, a small walnut-sized gland in men that produces fluids that nourish and protect sperm. Cancer occurs when abnormal cells in the prostate gland grow and multiply uncontrollably, forming a tumor.
Early-stage prostate cancer often has no symptoms. As the cancer progresses, symptoms may include:
– Difficulty starting or stopping the flow of urine
– Weak or interrupted flow of urine
– Frequent urination, especially at night
– Painful or burning urination
– Difficulty getting an erection
– Painful ejaculation
– Blood in urine or semen
The exact cause of prostate cancer is unknown, but risk factors include:
– Age (risk increases after 50)
– Family history (having a father or brother with prostate cancer)
– Race (African American men have a higher risk)
Men with the following risk factors should be screened regularly:
– Age 50 or older
– African American men
– Men with a family history of prostate cancer
– Men with a history of prostate issues (e.g., enlarged prostate)
Diagnosis typically involves:
– PSA (prostate-specific antigen) test: measures protein levels in blood
– Digital rectal exam (DRE): doctor examines the prostate gland manually
– Biopsy: tissue sample is taken from the prostate gland for examination
The PSA test measures the level of prostate-specific antigen (PSA) in the blood. Elevated PSA levels can indicate prostate issues, including cancer.
Treatment options depend on the stage and aggressiveness of the cancer:
– Surgery (prostatectomy): removal of the prostate gland
– Radiation therapy: high-energy rays to kill cancer cells
– Active surveillance: regular monitoring without immediate treatment
– Hormone therapy: reducing androgen hormones to slow cancer growth
A prostatectomy is a surgical procedure to remove the prostate gland. There are two main types:
– Radical prostatectomy: removes the entire prostate gland
– Laparoscopic prostatectomy: minimally invasive surgery using a laparoscope
Radiation therapy uses high-energy rays to kill cancer cells. There are two main types:
– External beam radiation therapy (EBRT): radiation is delivered from outside the body
– Brachytherapy: radiation is delivered from inside the body using implanted seeds
Active surveillance is a treatment approach that involves regular monitoring and testing, including PSA tests and biopsies, to track the progression of the cancer without immediate treatment.
While there is no sure way to prevent prostate cancer, a healthy diet and regular exercise may help reduce the risk.
The 5-year survival rate for prostate cancer is high, around 92%, due to early detection and effective treatment.
Yes, prostate cancer can recur after treatment. Regular monitoring and follow-up appointments with a doctor are essential to detect any recurrences early.
Men with risk factors should get screened annually, starting at age 50. Men without risk factors should discuss screening with their doctor.
The impact of prostate cancer treatment on fertility depends on the type of treatment. Surgery and radiation therapy may affect fertility, while hormone therapy may not. Men should discuss their fertility options with their doctor before treatment.
Ovarian cancer is a type of cancer that affects the ovaries, which are the organs that produce eggs in women. It occurs when abnormal cells in the ovaries grow and multiply uncontrollably, forming a tumor.
Early-stage ovarian cancer often has no symptoms. As the cancer progresses, symptoms may include:
– Abdominal pain or discomfort
– Bloating or swelling in the abdomen
– Pelvic pain or pressure
– Abnormal vaginal bleeding or discharge
– Difficulty eating or feeling full quickly
– Urinary frequency or urgency
The exact cause of ovarian cancer is unknown, but risk factors include:
– Genetic mutations (BRCA1 and BRCA2 genes)
– Family history of ovarian or breast cancer
– Reproductive issues (endometriosis, polycystic ovary syndrome)
– Hormone replacement therapy
Women with the following risk factors should be screened regularly:
– BRCA1 or BRCA2 genetic mutation
– Family history of ovarian or breast cancer
– Reproductive issues (endometriosis, polycystic ovary syndrome)
– Age 55 or older
Diagnosis typically involves:
– Pelvic exam: doctor examines the ovaries and uterus manually
– Ultrasound: uses sound waves to create images of the ovaries
– CA-125 blood test: measures protein levels in blood
– Biopsy: tissue sample is taken from the ovary for examination
The CA-125 test measures the level of a protein called cancer antigen 125 in the blood. Elevated levels can indicate ovarian cancer.
7. What are the treatment options for ovarian cancer?
Treatment options depend on the stage and aggressiveness of the cancer:
– Surgery: removes tumor, ovaries, fallopian tubes, and uterus
– Chemotherapy: drugs to kill cancer cells
– Radiation therapy: high-energy rays to kill cancer cells
– Targeted therapy: drugs to target specific cancer cells
The goal of surgery is to remove the tumor, ovaries, fallopian tubes, and uterus to prevent the cancer from spreading.
Chemotherapy uses drugs to kill cancer cells. It can be given orally or intravenously.
While there is no sure way to prevent ovarian cancer, birth control pills and tubal ligation may reduce the risk.
The 5-year survival rate for ovarian cancer is around 49%, depending on the stage and treatment.
Yes, ovarian cancer can recur after treatment. Regular monitoring and follow-up appointments with a doctor are essential.
Annual screening is recommended for high-risk women, including those with a family history or genetic mutation.
Depends on the type of treatment and individual situation. Some treatments may affect fertility.
Genetic testing identifies BRCA1 and BRCA2 genes, which increase ovarian cancer risk. Knowing your genetic status can help guide screening and prevention decisions.
Early detection improves treatment outcomes and survival rates. It also reduces the risk of complications and improves quality of life.
Cervical cancer is a type of cancer that affects the cervix, the lower part of the uterus (womb). It occurs when abnormal cells in the cervix grow and multiply uncontrollably, forming a tumor. Over time, the tumor can invade the surrounding tissues and spread to other parts of the body.
Early-stage cervical cancer often has no symptoms. However, as the cancer progresses, symptoms may include:
– Abnormal vaginal bleeding (e.g., bleeding between periods, after sex, or after menopause)
– Pelvic pain or discomfort
– Painful urination or defecation
– Unusual vaginal discharge (e.g., bloody, watery, or foul-smelling)
– Postcoital bleeding (bleeding after sexual intercourse)
– Unexplained weight loss
Women who have had sexual contact, have a weakened immune system, or have a history of cervical dysplasia (abnormal cell changes in the cervix) are at increased risk. Other risk factors include:
– Early sexual activity
– Multiple sexual partners
– Smoking
– Family history of cervical cancer
– History of other cancers (e.g., vulvar, vaginal, or anal cancer)
Diagnosis typically involves:
– Pap test (Pap smear): a procedure to collect cells from the cervix to check for abnormal cell changes
– HPV test: a test to check for the presence of HPV in the cervix
– Colposcopy: a procedure to examine the cervix with a special microscope
– Biopsy: a procedure to remove a tissue sample from the cervix for examination
A Pap test, also known as a Pap smear, is a procedure to collect cells from the cervix to check for abnormal cell changes. The test can detect:
– Normal cells
– Atypical cells (abnormal cells that may become cancerous)
– Cancer cells
The HPV test checks for the presence of HPV in the cervix. The test can detect:
– High-risk HPV types (e.g., HPV 16 and 18)
– Low-risk HPV types (e.g., HPV 6 and 11)
Treatment options depend on the stage and aggressiveness of the cancer and include:
– Surgery (e.g., hysterectomy, radical trachelectomy)
– Chemotherapy
– Radiation therapy
– Targeted therapy (e.g., bevacizumab)
– Immunotherapy (e.g., pembrolizumab)
The goal of surgery is to remove the tumor and affected tissue to prevent the cancer from spreading. The type of surgery depends on the stage and location of the cancer.
Yes, cervical cancer can be prevented with:
– Regular screening (Pap test and HPV test)
– HPV vaccination (e.g., Gardasil, Cervarix)
– Practicing safe sex (e.g., using condoms)
– Avoiding smoking and secondhand smoke
The 5-year survival rate for cervical cancer is around 66%, depending on the stage and treatment. Early detection improves survival rates.
Yes, cervical cancer can recur after treatment. Regular monitoring and follow-up appointments with a doctor are essential to detect any recurrences early.
Annual screening is recommended for women aged 21-65, or earlier if there is a history of cervical dysplasia or other risk factors.
Yes, most women can resume normal activities after treatment. However, some may experience lingering effects like vaginal dryness or painful urination.
Early detection improves treatment outcomes and survival rates. It also reduces the risk of complications and improves quality of life. Regular screening and HPV vaccination can help prevent cervical cancer and detect it early, when it is most treatable.
Oral cavity cancer, also known as mouth cancer, is a type of cancer that affects the oral cavity, including the lips, tongue, cheeks, floor of the mouth, and hard palate. It occurs when abnormal cells in the oral cavity grow and multiply uncontrollably, forming a tumor.
Early-stage oral cavity cancer often has no symptoms. As the cancer progresses, symptoms may include:
– Pain or difficulty swallowing
– Pain or difficulty speaking
– Pain or difficulty moving the tongue or jaw
– Unusual lumps or swelling in the mouth
– Unusual bleeding or pain in the mouth
– Loose teeth or dentures
– Difficulty chewing or swallowing
– Unusual changes in the voice
The main cause of oral cavity cancer is tobacco use, including smoking and chewing tobacco. Other risk factors include:
– Heavy alcohol consumption
– Human papillomavirus (HPV) infection
– Family history of oral cavity cancer
– Poor oral hygiene
– Poor diet
– Exposure to radiation therapy
Individuals who use tobacco, consume excessive alcohol, have a history of HPV infection, or have a family history of oral cavity cancer are at increased risk. Men are more likely to develop oral cavity cancer than women.
Diagnosis typically involves:
– Visual examination of the oral cavity
– Biopsy (removing a tissue sample for examination)
– Imaging tests (e.g., X-rays, CT scans, MRI scans)
Treatment options depend on the stage and aggressiveness of the cancer and include:
– Surgery (e.g., tumor resection, neck dissection)
– Radiation therapy
– Chemotherapy
– Targeted therapy
– Immunotherapy
The goal of surgery is to remove the tumor and affected tissue to prevent the cancer from spreading.
Yes, oral cavity cancer can be prevented by:
– Avoiding tobacco use
– Limiting alcohol consumption
– Practicing good oral hygiene
– Getting regular dental check-ups
– Avoiding exposure to radiation therapy
– Getting vaccinated against HPV
The 5-year survival rate for oral cavity cancer is around 66%, depending on the stage and treatment. Early detection improves survival rates.
Yes, oral cavity cancer can recur after treatment. Regular monitoring and follow-up appointments with a doctor are essential to detect any recurrences early.
Annual screening is recommended for individuals aged 18-65, or earlier if there is a history of oral cavity cancer or other risk factors.
Yes, most individuals can resume normal activities after treatment. However, some may experience lingering effects like difficulty speaking or swallowing.
Early detection improves treatment outcomes and survival rates. It also reduces the risk of complications and improves quality of life.
You can reduce your risk by avoiding tobacco use, limiting alcohol consumption, practicing good oral hygiene, getting regular dental check-ups, avoiding exposure to radiation therapy, and getting vaccinated against HPV.
You can get more information from your doctor, dentist, or organizations like the American Cancer Society, Oral Cancer Foundation, and National Institute of Dental and Craniofacial Research.
Blood cancer, also known as hematologic cancer, is a type of cancer that affects the blood and bone marrow. It occurs when abnormal cells in the blood or bone marrow grow and multiply uncontrollably, disrupting normal blood function.
– Leukemia (e.g., acute myeloid leukemia, chronic lymphocytic leukemia)
– Lymphoma (e.g., Hodgkin lymphoma, non-Hodgkin lymphoma)
– Multiple myeloma
– Myeloproliferative neoplasms (e.g., polycythemia vera, essential thrombocythemia)
– Myelodysplastic syndrome
– Leukemia: cancer of the white blood cells
– Lymphoma: cancer of the immune system
– Multiple myeloma: cancer of the plasma cells
– Myeloproliferative neoplasms: group of disorders that affect the bone marrow
– Myelodysplastic syndrome: condition where the bone marrow does not produce enough healthy blood cells
– Fatigue
– Shortness of breath
– Easy bruising or bleeding
– Pale skin
– Enlarged lymph nodes
– Unusual infections
– Weight loss
– Bone pain
– Abnormal blood cell counts
– Genetic mutations
– Exposure to radiation or chemicals
– Family history
– Previous cancer treatment
– Certain medical conditions (e.g., myelodysplastic syndrome)
– Individuals with a family history of blood cancer
– Previous cancer treatment
– Certain medical conditions (e.g., myelodysplastic syndrome)
– Genetic mutations
– Exposure to radiation or chemicals
– Physical examination
– Blood tests (e.g., complete blood count, blood chemistry tests)
– Bone marrow biopsy
– Imaging tests (e.g., X-rays, CT scans, PET scans)
– Chemotherapy
– Radiation therapy
– Targeted therapy
– Immunotherapy
– Stem cell transplantation
– Supportive care (e.g., blood transfusions, antibiotics)
– Control the cancer
– Manage symptoms
– Improve quality of life
– Cure the cancer (depending on the type and stage)
– Some types of blood cancer can be cured with treatment
– Others may require ongoing management
– Prognosis and potential for cure depend on the type and stage of cancer, as well as the individual’s overall health
– 5-year survival rate varies depending on the type and stage of cancer
– Ranges from around 20% to over 90%
– Yes, blood cancer can recur after treatment
– Regular monitoring and follow-up appointments with a doctor are essential
– Screening is not recommended for the general population
– Individuals with a family history or other risk factors may benefit from regular check-ups with their doctor
– Yes, many individuals can resume normal activities after treatment
– Some may experience lingering effects like fatigue or an increased risk of infections
– Improves treatment outcomes and survival rates
– Reduces the risk of complications and improves quality of life
– Your doctor or hematologist
– American Cancer Society
– Leukemia & Lymphoma Society
– National Cancer Institute
Anal cancer is a type of cancer that affects the anus, which is the opening at the end of the digestive tract. It occurs when abnormal cells in the anus grow and multiply uncontrollably, forming a tumor.
– Types of anal cancer:
– Squamous cell carcinoma
– Adenocarcinoma
– Basal cell carcinoma
– Melanoma
– Leukemia (e.g., acute myeloid leukemia, chronic lymphocytic leukemia)
– Lymphoma (e.g., Hodgkin lymphoma, non-Hodgkin lymphoma)
– Multiple myeloma
– Myeloproliferative neoplasms (e.g., polycythemia vera, essential thrombocythemia)
– Myelodysplastic syndrome
Symptoms of anal cancer may include:
– Bleeding from the anus or rectum
– Pain or discomfort in the anus or rectum
– Itching or irritation in the anus
– A lump or mass in the anus or rectum
– Changes in bowel movements (e.g., diarrhea, constipation)
– Discharge or pus from the anus
– Narrowing of the stool
The exact cause of anal cancer is unknown, but certain factors can increase the risk:
– Human papillomavirus (HPV) infection
– Anal sex
– Weakened immune system (e.g., HIV/AIDS, immunosuppressive therapy)
– History of cervical, vulvar, or vaginal cancer
– Smoking
– Age (risk increases after 50)
Individuals at risk for anal cancer include:
– Men who have sex with men
– Women with a history of cervical, vulvar, or vaginal cancer
– Individuals with a weakened immune system
– Those who engage in anal sex
– Smokers
– Individuals over 50
Diagnosis typically involves:
– Physical examination
– Digital rectal examination (DRE)
– Anoscopy (examining the inside of the anus with a scope)
– Biopsy (removing a tissue sample for examination)
– Imaging tests (e.g., CT scans, MRI scans)
Treatment options depend on the stage and location of the cancer:
– Surgery (e.g., local resection, abdominoperineal resection)
– Radiation therapy
– Chemotherapy
– Targeted therapy
– Immunotherapy
– Pain management
The goal of treatment is to:
– Remove the tumor
– Prevent the cancer from spreading
– Relieve symptoms
– Improve quality of life
– Cure the cancer (depending on the stage and location)
Yes, anal cancer can be cured with treatment, especially if detected early. The prognosis and potential for cure depend on the stage and location of the cancer, as well as the individual’s overall health.
The 5-year survival rate for anal cancer is around 65%, depending on the stage and location of the cancer.
Yes, anal cancer can recur after treatment. Regular monitoring and follow-up appointments with a doctor are essential to detect any recurrences early.
Screening is not recommended for the general population, but individuals at high risk (e.g., men who have sex with men, those with a history of cervical, vulvar, or vaginal cancer) may benefit from regular screening with a digital rectal examination (DRE) and anoscopy.
Yes, many individuals can resume normal activities after treatment, but some may experience lingering effects like pain, bleeding, or changes in bowel movements.
Early detection improves treatment outcomes and survival rates, and reduces the risk of complications and improves quality of life.
You can get more information from your doctor, a colorectal surgeon, or organizations like the American Cancer Society, the National Cancer Institute, and the Anal Cancer Foundation.
Support resources include:
– Counseling
– Support groups
– Online forums and communities
– Educational resources
– Financial assistance programs
Stomach cancer, also known as gastric cancer, is a type of cancer that affects the stomach. It occurs when abnormal cells in the stomach grow and multiply uncontrollably, forming a tumor.
– Types of stomach cancer:
– Adenocarcinoma
– Squamous cell carcinoma
– Lymphoma
– Gastrointestinal stromal tumor (GIST)
Symptoms of stomach cancer may include:
– Abdominal pain or discomfort
– Nausea and vomiting
– Weight loss
– Loss of appetite
– Bloating or gas
– Difficulty swallowing
– Blood in stool or vomit
– Fatigue
The exact cause of stomach cancer is unknown, but certain factors can increase the risk:
– Infection with Helicobacter pylori (H. pylori)
– Diet high in salt and processed meat
– Smoking
– Family history
– Age (risk increases after 50)
– Gender (men are more likely to develop stomach cancer)
– Obesity
– Pernicious anemia
– Radiation exposure
Individuals at risk for stomach cancer include:
– Those infected with H. pylori
– Men over 50
– Women over 60
– Individuals with a family history
– Smokers
– Those with a diet high in salt and processed meat
– Obese individuals
– Those with pernicious anemia
– Those exposed to radiation
Diagnosis typically involves:
– Endoscopy
– Upper gastrointestinal series (UGI)
– Computed tomography (CT) scan
– Magnetic resonance imaging (MRI) scan
– Positron emission tomography (PET) scan
– Biopsy
Treatment options depend on the stage and location of the cancer:
– Surgery (e.g., gastrectomy, subtotal gastrectomy)
– Chemotherapy
– Radiation therapy
– Targeted therapy
– Immunotherapy
– Palliative care
The goal of treatment is to:
– Remove the tumor
– Prevent the cancer from spreading
– Relieve symptoms
– Improve quality of life
– Cure the cancer (depending on the stage and location)
Yes, stomach cancer can be cured with treatment, especially if detected early. The prognosis and potential for cure depend on the stage and location of the cancer, as well as the individual’s overall health.
The 5-year survival rate for stomach cancer is around 30%, depending on the stage and location of the cancer.
Yes, stomach cancer can recur after treatment. Regular monitoring and follow-up appointments with a doctor are essential to detect any recurrences early.
Screening is not recommended for the general population, but individuals at high risk (e.g., those with H. pylori infection, family history, or previous stomach cancer) may benefit from regular screening with endoscopy and biopsy.
Yes, many individuals can resume normal activities after treatment, but some may experience lingering effects like pain, nausea, or changes in appetite.
Early detection improves treatment outcomes and survival rates, and reduces the risk of complications and improves quality of life.
You can get more information from your doctor, a gastroenterologist, or organizations like the American Cancer Society, the National Cancer Institute, and the Stomach Cancer Foundation.
Support resources include:
– Counseling
– Support groups
– Online forums and communities
– Educational resources
– Financial assistance programs
Esophageal cancer is a type of cancer that affects the esophagus, which is the tube that carries food and liquids from the throat to the stomach. It occurs when abnormal cells in the esophagus grow and multiply uncontrollably, forming a tumor.
– Types of esophageal cancer:
– Adenocarcinoma
– Squamous cell carcinoma
– Lymphoma
– Gastrointestinal stromal tumor (GIST)
Symptoms of esophageal cancer may include:
– Difficulty swallowing (dysphagia)
– Pain or discomfort in the chest or back
– Weight loss
– Coughing or choking on food
– Hoarseness
– Blood in stool or vomit
– Fatigue
The exact cause of esophageal cancer is unknown, but certain factors can increase the risk:
– Smoking
– Heavy alcohol consumption
– Gastroesophageal reflux disease (GERD)
– Barrett’s esophagus
– Family history
– Age (risk increases after 50)
– Gender (men are more likely to develop esophageal cancer)
– Obesity
– Diet high in processed meat and low in fruits and vegetables
Individuals at risk for esophageal cancer include:
– Smokers
– Heavy alcohol consumers
– Those with GERD or Barrett’s esophagus
– Men over 50
– Women over 60
– Obese individuals
– Those with a family history
– Those who eat a diet high in processed meat and low in fruits and vegetables
Diagnosis typically involves:
– Endoscopy
– Biopsy
– Computed tomography (CT) scan
– Magnetic resonance imaging (MRI) scan
– Positron emission tomography (PET) scan
– Barium swallow
Treatment options depend on the stage and location of the cancer:
– Surgery (e.g., esophagectomy, subtotal esophagectomy)
– Chemotherapy
– Radiation therapy
– Targeted therapy
– Immunotherapy
– Palliative care
The goal of treatment is to:
– Remove the tumor
– Prevent the cancer from spreading
– Relieve symptoms
– Improve quality of life
– Cure the cancer (depending on the stage and location)
Yes, esophageal cancer can be cured with treatment, especially if detected early. The prognosis and potential for cure depend on the stage and location of the cancer, as well as the individual’s overall health.
The 5-year survival rate for esophageal cancer is around 20%, depending on the stage and location of the cancer.
Yes, esophageal cancer can recur after treatment. Regular monitoring and follow-up appointments with a doctor are essential to detect any recurrences early.
Screening is not recommended for the general population, but individuals at high risk (e.g., those with GERD or Barrett’s esophagus) may benefit from regular screening with endoscopy and biopsy.
Yes, many individuals can resume normal activities after treatment, but some may experience lingering effects like difficulty swallowing or chest pain.
Early detection improves treatment outcomes and survival rates, and reduces the risk of complications and improves quality of life.
You can get more information from your doctor, a gastroenterologist, or organizations like the American Cancer Society, the National Cancer Institute, and the Esophageal Cancer Foundation.
Support resources include:
– Counseling
– Support groups
– Online forums and communities
– Educational resources
– Financial assistance programs
Gallbladder cancer is a type of cancer that affects the gallbladder, a small organ located under the liver that stores bile. It occurs when abnormal cells in the gallbladder grow and multiply uncontrollably, forming a tumor.
– Types of gallbladder cancer:
– Adenocarcinoma
– Squamous cell carcinoma
– Adenosquamous carcinoma
– Sarcoma
Symptoms of gallbladder cancer may include:
– Abdominal pain (especially in the right upper quadrant)
– Nausea and vomiting
– Weight loss
– Loss of appetite
– Jaundice (yellowing of the skin and eyes)
– Pale or clay-colored stools
– Dark urine
– Fever
– Shaking chills
The exact cause of gallbladder cancer is unknown, but certain factors can increase the risk:
– Gallstones
– Choledochal cysts
– Primary sclerosing cholangitis
– Ulcerative colitis
– Family history
– Age (risk increases after 50)
– Gender (women are more likely to develop gallbladder cancer)
– Obesity
– Diabetes
– High cholesterol
Individuals at risk for gallbladder cancer include:
– Those with a history of gallstones
– Those with choledochal cysts
– Those with primary sclerosing cholangitis
– Those with ulcerative colitis
– Women over 50
– Obese individuals
– Those with diabetes
– Those with high cholesterol
– Those with a family history
Diagnosis typically involves:
– Physical examination
– Medical history
– Laboratory tests (e.g., liver function tests, tumor markers)
– Imaging tests (e.g., ultrasound, CT scan, MRI scan)
– Biopsy
Treatment options depend on the stage and location of the cancer:
– Surgery (e.g., cholecystectomy, radical cholecystectomy)
– Chemotherapy
– Radiation therapy
– Targeted therapy
– Immunotherapy
– Palliative care
The goal of treatment is to:
– Remove the tumor
– Prevent the cancer from spreading
– Relieve symptoms
– Improve quality of life
– Cure the cancer (depending on the stage and location)
Yes, gallbladder cancer can be cured with treatment, especially if detected early. The prognosis and potential for cure depend on the stage and location of the cancer, as well as the individual’s overall health.
The 5-year survival rate for gallbladder cancer is around 20%, depending on the stage and location of the cancer.
Yes, gallbladder cancer can recur after treatment. Regular monitoring and follow-up appointments with a doctor are essential to detect any recurrences early.
Screening is not recommended for the general population, but individuals at high risk (e.g., those with gallstones or choledochal cysts) may benefit from regular screening with ultrasound and laboratory tests.
Yes, many individuals can resume normal activities after treatment, but some may experience lingering effects like abdominal pain or jaundice.
Early detection improves treatment outcomes and survival rates, and reduces the risk of complications and improves quality of life.
You can get more information from your doctor, a gastroenterologist, or organizations like the American Cancer Society, the National Cancer Institute, and the Gallbladder Cancer Foundation.
Support resources include:
– Counseling
– Support groups
– Online forums and communities
– Educational resources
– Financial assistance programs
Urinary bladder cancer is a type of cancer that affects the urinary bladder, a hollow organ that stores urine. It occurs when abnormal cells in the bladder grow and multiply uncontrollably, forming a tumor.
– Types of urinary bladder cancer:
– Transitional cell carcinoma (TCC)
– Squamous cell carcinoma (SCC)
– Adenocarcinoma
– Sarcoma
Symptoms of urinary bladder cancer may include:
– Blood in the urine (hematuria)
– Painful urination (dysuria)
– Frequent urination
– Urgent need to urinate
– Pain in the lower abdomen or back
– Weakness or fatigue
– Loss of appetite
– Weight loss
The exact cause of urinary bladder cancer is unknown, but certain factors can increase the risk:
– Smoking
– Exposure to chemicals (e.g., benzene, arsenic)
– Radiation therapy
– Family history
– Age (risk increases after 50)
– Gender (men are more likely to develop bladder cancer)
– Race (whites are more likely to develop bladder cancer)
– Chronic bladder inflammation
– Bladder birth defects
Individuals at risk for urinary bladder cancer include:
– Smokers
– Those exposed to chemicals (e.g., benzene, arsenic)
– Those with a family history
– Men over 50
– Women over 50
– Whites
– Those with chronic bladder inflammation
– Those with bladder birth defects
Diagnosis typically involves:
– Physical examination
– Medical history
– Laboratory tests (e.g., urinalysis, blood tests)
– Imaging tests (e.g., ultrasound, CT scan, MRI scan)
– Cystoscopy
– Biopsy
Treatment options depend on the stage and location of the cancer:
– Surgery (e.g., transurethral resection of bladder tumor, radical cystectomy)
– Chemotherapy
– Radiation therapy
– Immunotherapy
– Targeted therapy
– Palliative care
The goal of treatment is to:
– Remove the tumor
– Prevent the cancer from spreading
– Relieve symptoms
– Improve quality of life
– Cure the cancer (depending on the stage and location)
Yes, urinary bladder cancer can be cured with treatment, especially if detected early. The prognosis and potential for cure depend on the stage and location of the cancer, as well as the individual’s overall health.
The 5-year survival rate for urinary bladder cancer is around 70%, depending on the stage and location of the cancer.
Yes, urinary bladder cancer can recur after treatment. Regular monitoring and follow-up appointments with a doctor are essential to detect any recurrences early.
Screening is not recommended for the general population, but individuals at high risk (e.g., those with a history of smoking or exposure to chemicals) may benefit from regular screening with urinalysis and cystoscopy.
Yes, many individuals can resume normal activities after treatment, but some may experience lingering effects like urinary incontinence or sexual dysfunction.
Early detection improves treatment outcomes and survival rates, and reduces the risk of complications and improves quality of life.
You can get more information from your doctor, a urologist, or organizations like the American Cancer Society, the National Cancer Institute, and the Bladder Cancer Foundation.
Support resources include:
– Counseling
– Support groups
– Online forums and communities
– Educational resources
– Financial assistance programs
Bone cancer is a type of cancer that affects the bones. It occurs when abnormal cells in the bone grow and multiply uncontrollably, forming a tumor.
– Types of bone cancer:
– Osteosarcoma
– Ewing’s sarcoma
– Chondrosarcoma
– Fibrosarcoma
– Chordoma
Symptoms of bone cancer may include:
– Pain in the affected bone
– Swelling or redness in the affected area
– Weakness or fatigue
– Difficulty moving the affected limb
– Fractures or breaks in the affected bone
– Weight loss
– Fever
– Night sweats
The exact cause of bone cancer is unknown, but certain factors can increase the risk:
– Genetic mutations
– Family history
– Radiation exposure
– Chemotherapy
– Certain bone diseases (e.g., Paget’s disease, osteochondritis)
– Inherited conditions (e.g., Li-Fraumeni syndrome, hereditary multiple exostoses)
Individuals at risk for bone cancer include:
– Those with a family history
– Those with genetic mutations
– Those who have had radiation therapy
– Those with certain bone diseases
– Those with inherited conditions
– Children and young adults (bone cancer is more common in this age group)
Diagnosis typically involves:
– Physical examination
– Medical history
– Laboratory tests (e.g., blood tests, imaging studies)
– Biopsy
Treatment options depend on the type and stage of the cancer:
– Surgery (e.g., limb-sparing surgery, amputation)
– Chemotherapy
– Radiation therapy
– Targeted therapy
– Immunotherapy
– Palliative care
The goal of treatment is to:
– Remove the tumor
– Prevent the cancer from spreading
– Relieve symptoms
– Improve quality of life
– Cure the cancer (depending on the type and stage)
Yes, bone cancer can be cured with treatment, especially if detected early. The prognosis and potential for cure depend on the type and stage of the cancer, as well as the individual’s overall health.
The 5-year survival rate for bone cancer is around 70%, depending on the type and stage of the cancer.
Yes, bone cancer can recur after treatment. Regular monitoring and follow-up appointments with a doctor are essential to detect any recurrences early.
Screening is not recommended for the general population, but individuals at high risk (e.g., those with a family history or genetic mutation) may benefit from regular screening with imaging studies and laboratory tests.
Yes, many individuals can resume normal activities after treatment, but some may experience lingering effects like limited mobility or chronic pain.
Early detection improves treatment outcomes and survival rates, and reduces the risk of complications and improves quality of life.
You can get more information from your doctor, an orthopedic oncologist, or organizations like the American Cancer Society, the National Cancer Institute, and the Bone Cancer Foundation.
Support resources include:
– Counseling
– Support groups
– Online forums and communities
– Educational resources
– Financial assistance programs
Pancreatic cancer is a type of cancer that affects the pancreas, an organ located in the abdomen that produces hormones and enzymes to aid in digestion. It occurs when abnormal cells in the pancreas grow and multiply uncontrollably, forming a tumor.
– Types of pancreatic cancer:
– Adenocarcinoma
– Squamous cell carcinoma
– Neuroendocrine tumors (NETs)
– Pancreatic neuroendocrine tumors (PNETs)
Symptoms of pancreatic cancer may include:
– Abdominal pain or discomfort
– Weight loss
– Loss of appetite
– Fatigue
– Jaundice (yellowing of the skin and eyes)
– Dark urine
– Pale or clay-colored stools
– Nausea and vomiting
– Diarrhea or constipation
– Blood clots
The exact cause of pancreatic cancer is unknown, but certain factors can increase the risk:
– Smoking
– Family history
– Age (risk increases after 50)
– Gender (men are more likely to develop pancreatic cancer)
– Race (African Americans are more likely to develop pancreatic cancer)
– Obesity
– Diabetes
– Pancreatitis (inflammation of the pancreas)
– Genetic mutations (e.g., BRCA2, p16)
Individuals at risk for pancreatic cancer include:
– Smokers
– Those with a family history
– Men over 50
– African Americans
– Obese individuals
– Those with diabetes
– Those with pancreatitis
– Those with genetic mutations
Diagnosis typically involves:
– Physical examination
– Medical history
– Laboratory tests (e.g., blood tests, imaging studies)
– Biopsy
Treatment options depend on the stage and location of the cancer:
– Surgery (e.g., Whipple procedure, distal pancreatectomy)
– Chemotherapy
– Radiation therapy
– Targeted therapy
– Immunotherapy
– Palliative care
The goal of treatment is to:
– Remove the tumor
– Prevent the cancer from spreading
– Relieve symptoms
– Improve quality of life
– Cure the cancer (depending on the stage and location)
Yes, pancreatic cancer can be cured with treatment, especially if detected early. The prognosis and potential for cure depend on the stage and location of the cancer, as well as the individual’s overall health.
The 5-year survival rate for pancreatic cancer is around 9%, depending on the stage and location of the cancer.
Yes, pancreatic cancer can recur after treatment. Regular monitoring and follow-up appointments with a doctor are essential to detect any recurrences early.
Screening is not recommended for the general population, but individuals at high risk (e.g., those with a family history or genetic mutation) may benefit from regular screening with imaging studies and laboratory tests.
Yes, many individuals can resume normal activities after treatment, but some may experience lingering effects like digestive problems or fatigue.
Early detection improves treatment outcomes and survival rates, and reduces the risk of complications and improves quality of life.
You can get more information from your doctor, a gastroenterologist, or organizations like the American Cancer Society, the National Cancer Institute, and the Pancreatic Cancer Action Network.
Support resources include:
– Counseling
– Support groups
– Online forums and communities
– Educational resources
– Financial assistance programs